Introduction about Sleep
This page is designed to provide basic concepts and information about sleep.
For explanations of the sleep data provided by SleepTrack, please refer to the main concept pages.
Sleep stages
Until 1950s sleep was simply regarded as the opposite of “being awake.” Recent discoveries have changed the understanding of sleep to more complicated physiological processes. Sleep stages go through 90-minute intervals and are largely broken down into REM (Rapid Eye Movement) and NREM (non-REM) sleep. NREM sleep is, then consisted of light and deep sleeps.
Wake
Most adults are awake for two-thirds of the day. Having eyes open, conversing with others and moving around are all signs of being awake. Once we get ready for sleep, alpha rhythm in brainwave starts to be detected. The brainwave slows down even further and sleep arrives. Muscles relax and the eye movement slows down.
Light
We can get easily awaken from light sleep. Light sleep is the transition from wakefulness to sleep. Muscles relaxe, and eye movement and breathing slow down. Also, body temperature starts to fall. Because we spend most part of our sleep in light stage, light stage is as important as any other stage in sleep.
Deep
Deep sleep, also known as slow wave sleep, usually occurs in the first half of sleep. This is when eye and muscle movements stop, and slow brainwave starts. Our bodies recover and growth happens during this sleep stage. It is more difficult to be awaken up during deep sleep than light sleep.
REM (Rapid Eye Movement)
Rapid eye movements are the defining feature of the stage. This sleep stage appears after 90 minutes of falling asleep. The breathing becomes irregular and heart rate and blood pressure increase. At the same time, arm and leg muscles paralyze temporarily. REM sleep has typically been associated with vivid dreaming while memory gets consolidated and mood is stabilized.
Non-REM vs. REM
NREM | REM | |
|---|---|---|
Cardiovascular system | Heart rate is slow and regular | Heart rate is irregular |
Temperature regulation | Decreased hypothalamic temperature set point | Reduced thermoregulatory mechanisms |
Dreaming | Less vivid | More vivid, visually intense |
Sleep Stage | Light, Deep | REM |
- In sleep medicine, light sleep includes NREM(Non-Rapid Eye Movement) 1, 2 while deep sleep indicates NREM 3.
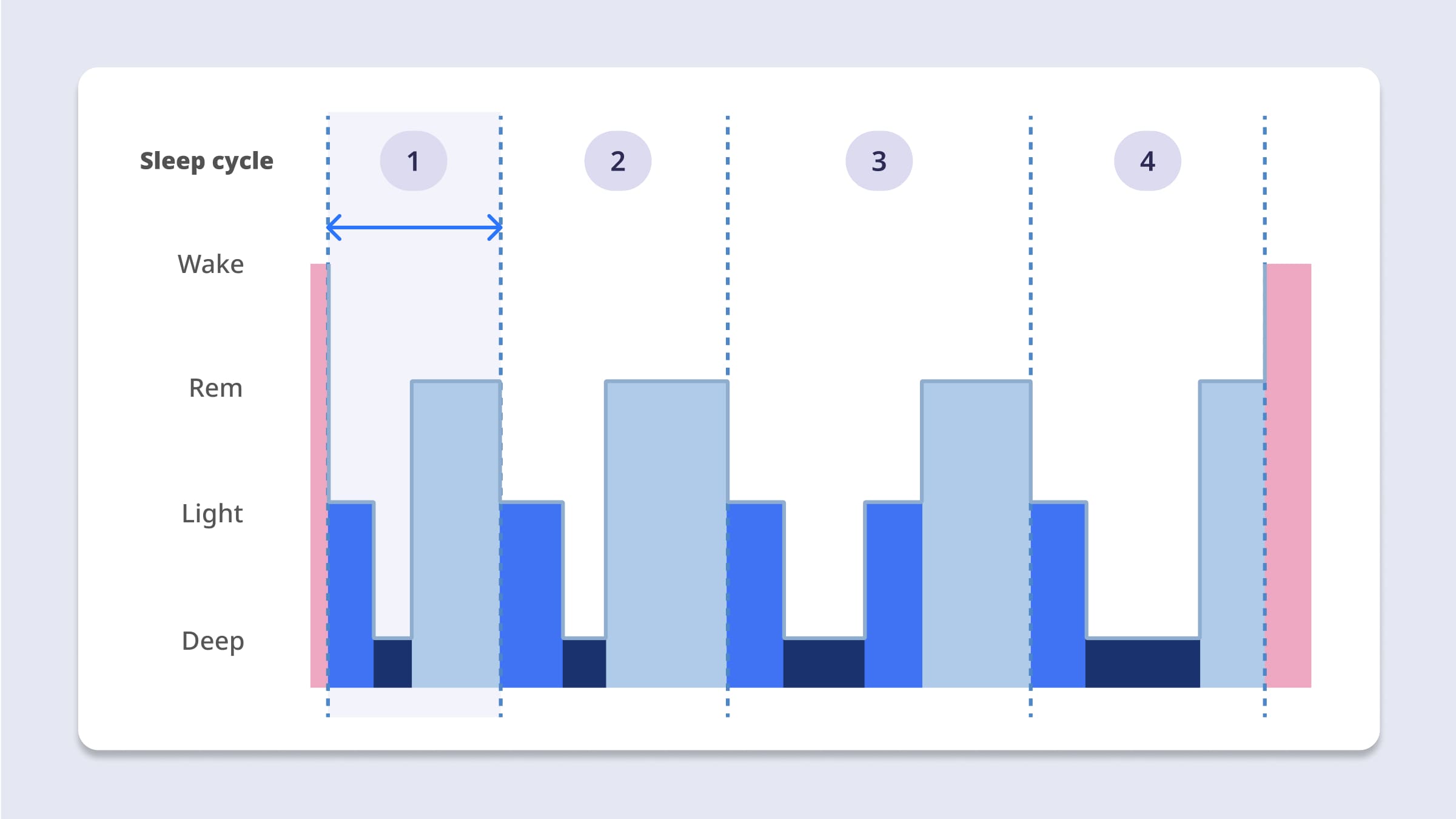
Sleep cycle
*The Sleep Cycle Data was released in beta on October 31, 2023.
During 8 hours of sleep, a healthy adult goes through about 4 to 5 sleep cycles per night. One sleep cycle lasts 90-120 minutes and is consisted of Non-Rapid Eye Movement (NREM) sleep and Rapid Eye Movement (REM) sleep. As an example, the first sleep cycle will typically encompass the time from initial sleep onset until the person exits from the first REM period.
Sleep cycles trend through a standard night in the following ways:
- The first cycle of the night starts with transition from wake to light sleep, then into deep sleep, and then REM.
- As the cycles continue during the night, the percentage of REM sleep in each cycle generally increases.
- The percentage of deep sleep tends to decrease over the course of the night, with the largest amount of deep sleep in the first half of the night.
Potential functions of sleep

Sleep is essential for brain function and physiologic health in a variety of ways.
Restorative function
A restorative theory proposes that the body repairs and revitalizes itself during the sleep state. Upon awakening from a full night of sleep, people typically feel restored. On the other hand, insufficient sleep results in poorer daytime performance, a feeling of tiredness or sleepiness, and measurable effects on immune function. Growth hormone is also secreted during sleep; this may contribute to muscle growth and cell regeneration during the night.
Clearance function
Brain metabolism during sleep is supposed to play a restorative function via clearance of substances such as adenosine. Adenosine builds up over the course of the day and helps to induce deep sleep.
Brain plasticity and learning
Brain plasticity is the ability of neural networks in the brain to change through growth and reorganization. And sleep is believed to play an important role in brain plasticity. Humans clearly learn less well when not sleeping enough; thus sleep must have an impact on cognitive function and memory.
Sleep hygiene
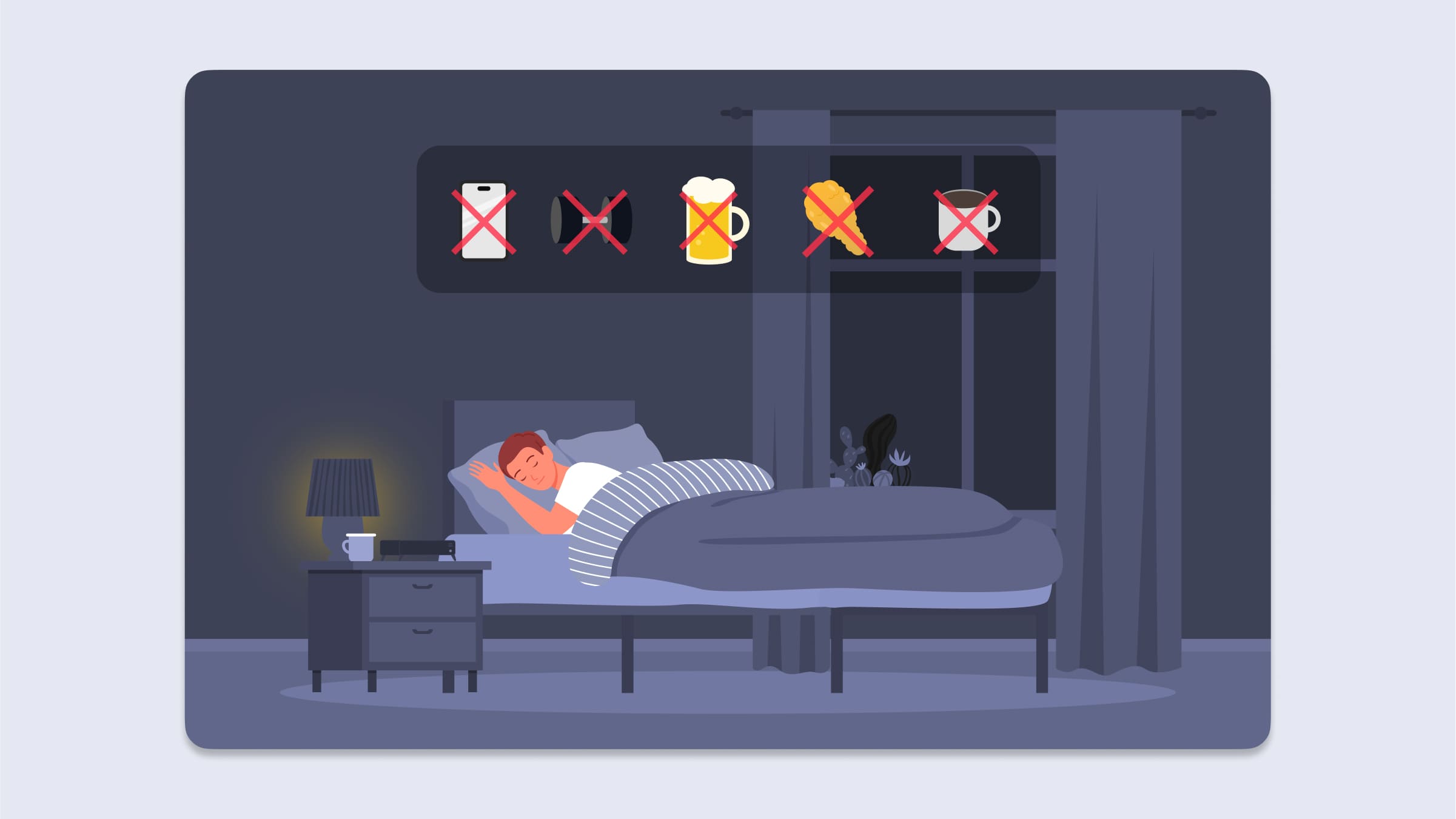
Sleep hygiene refers to a series of habits and environmental factors to achieve good sleep. It is important to create an optimal environment where both body and mind can rest to improve sleep quality. Maintaining good sleep hygiene is important not just for sleeping longer, but also for reaching optimal productivity. The following guidelines can help you fall asleep faster at night, promote deep sleep, and improve overall health and quality of daily life.
- Go to bed and get up at about the same time every day.
- Have coffee, tea, and other drinks or foods with caffeine until early in the afternoon.
- Avoid eating close to bedtime. Try to avoid late-night snacking.
- Avoid alcohol in the late afternoon, evening, and bedtime.
- Avoid smoking, especially in the evening.
- Keep your bedroom dark, cool, quiet, and free of reminders of work or other things that cause you stress.
- Try to solve problems before you go to bed.
- Get plenty of physical activity, but not right before bed. Exercising 4 to 6 hours before bedtime has the best impact on sleep.
- Avoid looking at phones or reading devices ("e-books") that give off light before bed.
- Avoid long naps in the late afternoon. Short naps (about 20 minutes) can be helpful, especially if your work schedule changes day to day and you need to be alert at different times.
Polysomnogram
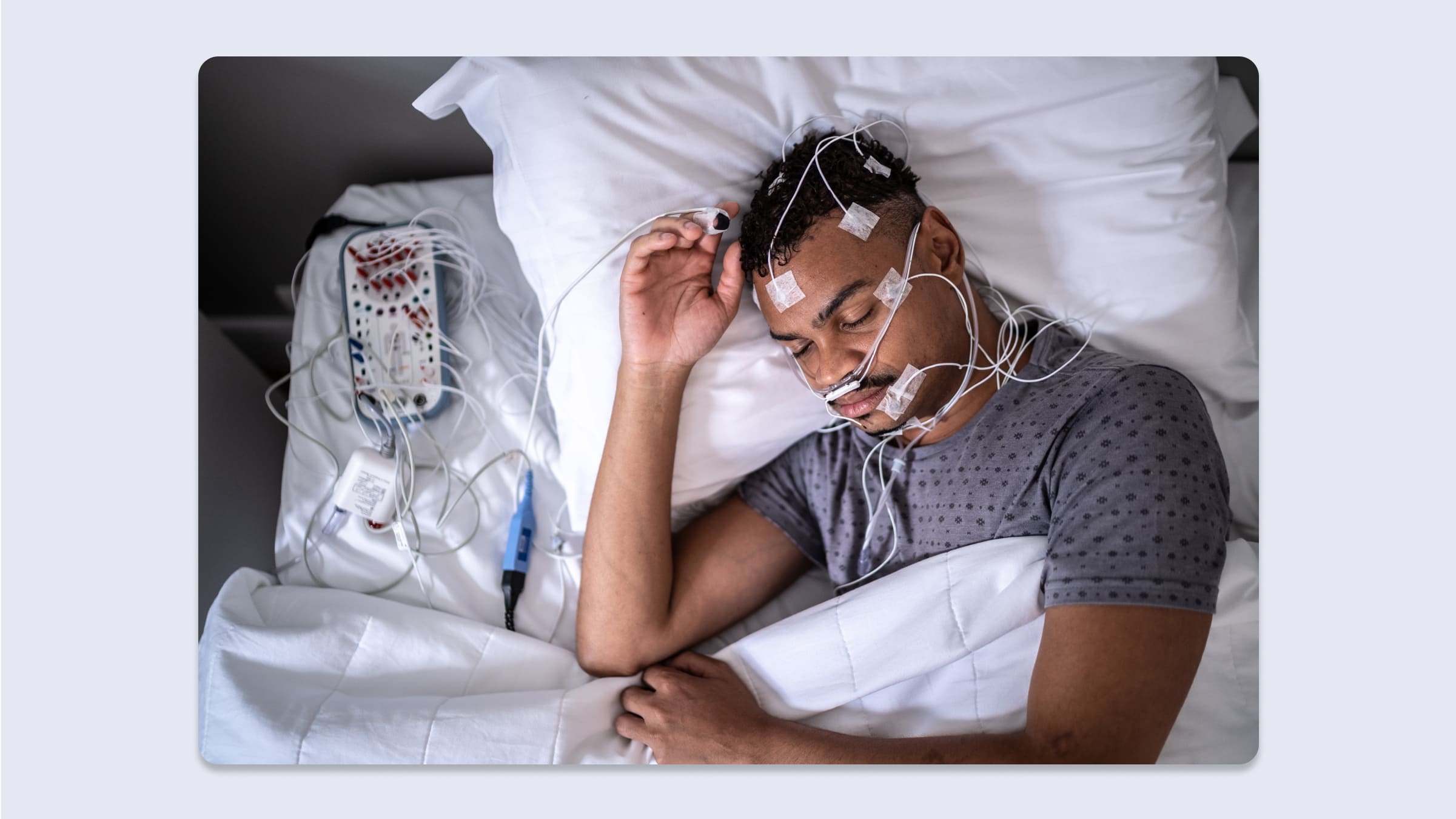
Polysomnography, or a sleep study, is a comprehensive diagnostic method that evaluates various physiological changes occurring during sleep to diagnose sleep disorders. This test is particularly important in assessing sleep-related breathing disorders like obstructive sleep apnea, abnormal behaviors during sleep, and issues related to the quality and structure of sleep. Polysomnography involves collecting a variety of physiological data during a night of natural sleep. This data provides a deep understanding of sleep quality, breathing issues during sleep, and heart and muscle activity. Such information is essential for medical professionals to diagnose sleep disorders and plan their treatment. Next, we will explain the specific methods, clinical applications, measured variables, and sleep-related information that can be obtained from polysomnography.
Technique
Attended, in-laboratory polysomnography (PSG) is considered the gold standard diagnostic test for obstructive sleep apnea (OSA) and other sleep disorders. During PSG, the patient sleeps while connected to numerous monitoring devices and a technologist records physiologic variables. Patterns of physiologic abnormalities during sleep are often diagnostic.
Indications
Diagnostic evaluation of suspected OSA, titration of positive airway pressure therapy, and assessment of the effectiveness of therapy are the most common indications for PSG. There are no contraindications to PSG and few complications, although patients should be medically stable to undergo the procedure.
Measured variables
Physiologic variables assessed during PSG include sleep stages, respiratory effort, airflow, blood saturation, electrocardiography, body position, and limb movements.
Derived information
From these physiologic variables, an abundance of information is derived. This includes sleep architecture, the frequency of abnormal events during sleep, and various diagnostic measures.
Updated 4 months ago
